Bone density testing in clients with post-polio syndrome has demonstrated the prevalence, risk factors, and management of osteoporosis in this population, highlighting the significance of bone health in post-polio syndrome.
This article delves into the rationale, methods, and interpretation of bone density testing, providing valuable insights into osteoporosis prevalence, risk factors, and the impact on health and well-being.
Bone Density Testing in Clients with Post-Polio Syndrome

Rationale for Conducting Bone Density Testing
Individuals with post-polio syndrome (PPS) have an increased risk of developing osteoporosis due to several factors, including muscle weakness, decreased mobility, and hormonal imbalances. Bone density testing is essential for identifying individuals at risk and monitoring the effectiveness of osteoporosis management strategies.
Methods Used to Perform Bone Density Testing
- Dual-energy X-ray absorptiometry (DXA) is the preferred method for measuring bone density in clients with PPS.
- Quantitative computed tomography (QCT) may be used to assess bone density in specific areas, such as the spine or hip.
Interpretation of Bone Density Test Results
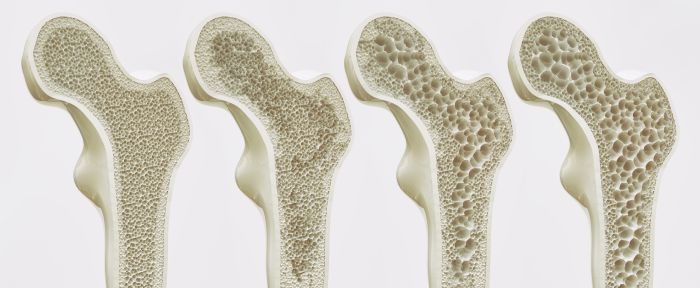
Bone density test results are interpreted using T-scores, which compare the individual’s bone density to the average peak bone density of healthy young adults. A T-score of -2.5 or lower is considered osteoporotic, while a T-score between -1.0 and -2.5 indicates osteopenia.
Prevalence and Risk Factors for Osteoporosis in Clients with Post-Polio Syndrome
Prevalence of Osteoporosis
Studies have shown that the prevalence of osteoporosis in clients with PPS ranges from 20% to 50%, significantly higher than the general population.
Risk Factors for Osteoporosis
- Age
- Female sex
- Muscle weakness
- Decreased mobility
- Hormonal imbalances
- Nutritional deficiencies
- Use of certain medications (e.g., corticosteroids)
Potential Impact of Osteoporosis
Osteoporosis can lead to increased risk of fractures, which can result in pain, disability, and reduced quality of life.
Management of Osteoporosis in Clients with Post-Polio Syndrome: Bone Density Testing In Clients With Post-polio Syndrome Has Demonstrated

Principles of Osteoporosis Management
The management of osteoporosis in clients with PPS focuses on preventing fractures and maintaining bone health. This includes:
- Lifestyle modifications (e.g., exercise, nutrition, fall prevention)
- Medication (e.g., bisphosphonates, denosumab)
- Other interventions (e.g., physical therapy, assistive devices)
Lifestyle Modifications
- Exercise:Regular weight-bearing exercise can help maintain bone density and reduce the risk of falls.
- Nutrition:Adequate intake of calcium and vitamin D is essential for bone health.
- Fall Prevention:Measures such as home modifications, assistive devices, and balance exercises can reduce the risk of falls.
Medication
- Bisphosphonates:These medications help prevent bone breakdown and increase bone density.
- Denosumab:This medication inhibits bone resorption and is used to treat osteoporosis in postmenopausal women.
Other Interventions
- Physical Therapy:Physical therapy can help improve mobility and reduce the risk of falls.
- Assistive Devices:Devices such as canes, walkers, and wheelchairs can provide support and improve mobility.
Multidisciplinary Approach to Bone Health in Clients with Post-Polio Syndrome

Benefits of a Multidisciplinary Approach
A multidisciplinary approach to bone health management in clients with PPS involves collaboration between different healthcare professionals, including:
- Physicians
- Nurses
- Physical therapists
- Occupational therapists
- Dietitians
This approach ensures that all aspects of bone health are addressed, including medical management, lifestyle modifications, and rehabilitation.
Patient Education and Empowerment
Patient education and empowerment are crucial for promoting bone health in clients with PPS. Healthcare professionals should provide information on:
- Osteoporosis and its risk factors
- Bone density testing and interpretation of results
- Lifestyle modifications and their importance
- Medication options and potential side effects
- Fall prevention strategies
Essential Questionnaire
What is the rationale for conducting bone density testing in clients with post-polio syndrome?
Bone density testing is crucial in this population due to the increased risk of osteoporosis and the potential impact of osteoporosis on mobility and overall health.
How is bone density testing performed in clients with post-polio syndrome?
Bone density testing is typically performed using dual-energy X-ray absorptiometry (DXA) scans, which measure bone mineral density in the spine, hip, and forearm.
What are the risk factors for osteoporosis in clients with post-polio syndrome?
Risk factors include age, female sex, low body weight, decreased physical activity, and certain medications, such as corticosteroids.